A skin cancer diagnosis can bring a lot of questions. AHN’s highly trained and experienced physicians are here to see you through tailored treatment options so you get the care you need.

What is skin cancer?
Skin cancer is one the most common types of cancers. It affects more than 3 million Americans each year. Knowing the most common types — basal cell carcinoma, squamous cell carcinoma, and melanoma — can help you feel knowledgeable about your treatment options and ensures an early diagnosis that can help in survival.
We work closely with Carnegie Mellon University to develop novel imaging technologies to catch skin cancer at its earliest stages. We use a pioneering process called sentinel lymph node mapping to help diagnose advanced cases of melanoma and certain high-risk squamous cell cancers.
At AHN Cancer Institute, we specialize in early detection and use targeted, minimally invasive treatments that protect the healthy skin tissue surrounding a tumor. Your whole health is taken into consideration when planning treatment. This means you are not only receiving care that is tailored to your specific diagnosis, but that care extends to your emotional health through comprehensive support resources.
Skin Cancer Center of Excellence
The AHN Skin Cancer Center of Excellence is at the forefront of delivering state-of-the art treatment for skin cancer and melanoma. No other skin cancer center in the area has the technology, care, and compassion that AHN provides to its patients.
Why choose AHN for skin cancer treatment
Although skin cancer is common, a diagnosis can be frightening. Remember, at the Cancer Institute, you’re never alone. We see you as a person and a patient who requires specific care that’s designed for your unique needs. You will find treatment that is:
- Personalized: Our skilled team of dermatologists, oncologists, dermatopathologists, and surgeons offer the latest targeted, minimally invasive surgeries or therapies tailored to the type of skin cancer you have.
- Patient-centric: Our Navigation Team helps coordinate appointments, answers questions about symptoms and treatment options, and provides logistical support if you need to travel. We help lift the burden of care planning so you can focus on getting better.
- Compassionate: Cancer treatment is a stressful time. Our compassionate team of caregivers is devoted to improving your quality of life, helping you understand treatment options, and keeping you comfortable every step of the way. Our robust support services help you live the best quality of life during treatment.
- Collaborative: Your treatment team works together to identify the right treatment for you, whether it’s surgery, medical oncology, or radiation therapy.

Skin cancer symptoms and signs
It’s easy to assume a skin lesion or a mole is harmless. However, it’s important to take note of skin changes or new spots that look suspicious or different. Skin cancer signs and symptoms vary for each person, but there are some key things to look out for. While basal and squamous cell cancer tend to grow slowly, melanoma can be more aggressive.
It is critical to receive an early, accurate diagnosis. A precise diagnosis helps to create an effective treatment plan that will give you the best long-term results. Reach out to your dermatologist or primary care provider right away if you suspect a change with your skin.
Skin cancer risk factors
Skin cancer is a serious disease, but understanding the risks can help you take steps to protect yourself.
- Excessive sun exposure: The primary culprit is ultraviolet (UV) radiation from the sun. Both UVA and UVB rays can damage DNA in skin cells, leading to cancer.
- Sunburns: Frequent sunburns, especially in childhood, significantly increase the risk of developing skin cancer later in life.
- Tanning beds and lamps: These devices emit high levels of UV radiation, posing a similar risk to sun exposure.
- Atypical moles: Moles that are unusual in size, shape, or color can be more prone to becoming cancerous.
- Precancerous lesions: Conditions like actinic keratosis can develop into skin cancer if left untreated.
- Fair skin: People with fair skin, freckles, and light hair are more susceptible to skin cancer due to lower melanin levels, which provide natural protection from UV radiation.
- Age: The risk of skin cancer increases with age, as cumulative sun exposure takes its toll.
- Medical conditions: Conditions like HIV/AIDS or organ transplantation can suppress the immune system, making it harder to fight off skin cancer cells.
- Medications: Certain medications, like immunosuppressants, can also weaken the immune system.
- Smoking: Smoking increases the risk of squamous cell carcinoma, a type of skin cancer.
- Alcohol consumption: Excessive alcohol consumption can also increase the risk of skin cancer.
- Outdoor workers: People who work outdoors for extended periods are at higher risk due to prolonged sun exposure.
- Certain industries: Workers in industries like construction, agriculture, fishing, aircrews, and firefighters are exposed to higher levels of UV radiation.
Skin cancer screening and diagnosis
Early cancer detection saves lives. We offer monthly cancer screenings across Pennsylvania so you can find resources and access where and when you need.
Basal and squamous cell cancers are almost always curable when we detect them early. Melanoma is more aggressive and can be life-threatening, so early detection is essential.
A physical exam
A physician, often a dermatologist, examines your skin to look for suspicious growths. Basal cell carcinomas often look pink, pearly, or pimple-like and squamous cell carcinomas tend to be tender and look red and flaky. Melanomas are usually atypical moles presenting with dark brown or black with multiple colors. Your doctor will use different techniques and procedures to get a comprehensive overview of your skin and any risks.
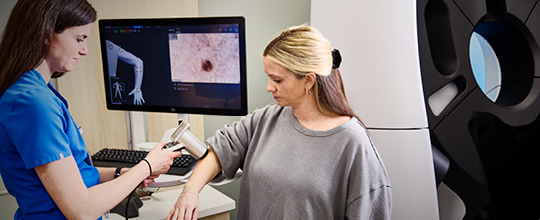
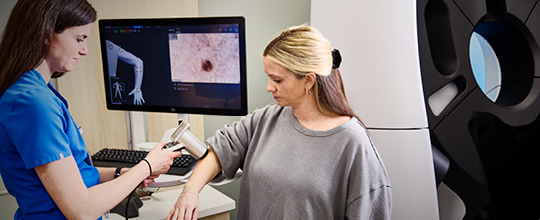
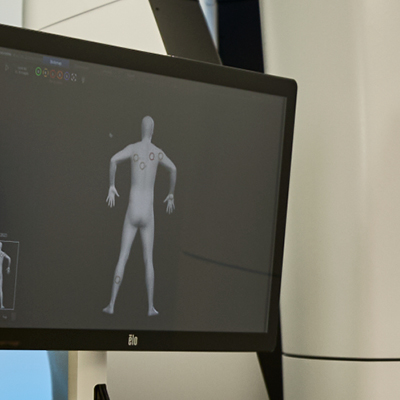
Mole mapping
This procedure uses full-body photographs of your skin to monitor changes in existing moles and to detect new ones. Physicians use this cutting-edge preventive measure at your annual skin exam. It’s especially helpful for tracking moles for high-risk individuals, such as those with a family history of melanoma.

Biopsy
A small tissue sample is collected to be examined by pathologist who specializes in dermatology. A biopsy can determine if cancer is present. During a biopsy, an anesthetic is given so the sample can be collected comfortably.
Biopsy procedures include:
- Shave biopsy, using a tool similar to a razor
- Punch biopsy, using a circular tool that removes a small section of skin
- Excisional biopsy, using a scalpel to remove an entire lump
Sentinel lymph node mapping
Sentinel lymph node mapping is a surgical technique used to determine if cancer has spread from the primary tumor to nearby lymph nodes. In a skin cancer diagnosis, specialists use this minimally invasive melanoma diagnostic tool to remove a sentinel node near cancerous tissues. The sample goes to a pathologist who specializes in skin cancer to determine if the node contains cancer cells and if the cancer has spread. Right now, we are using this for melanoma and other aggressive skin cancers including Merkel cell carcinoma. Our researchers are pioneering this technique for squamous cell cancer as well.
Types of skin cancer
Early detection and treatment are key in successfully managing a skin cancer diagnosis. Staying aware of skin changes is the easiest way to spot potential issues early. If you notice any unusual changes in your skin, consult a dermatologist immediately.
Skin cancer is broadly categorized as non-melanoma or melanoma.
Non-melanoma skin cancers are the most common type of skin cancer, accounting for the vast majority of cases. They are generally slow-growing and less aggressive than melanoma.
Melanoma is a less common but much more dangerous type of skin cancer. It can spread quickly to other parts of the body if not detected and treated early.
Non-melanoma skin cancer types
Both basal cell carcinoma and squamous cell carcinoma are non-melanoma skin cancer types.
Basal cell carcinoma (BCC)
The most common type, usually appearing as a pearly or waxy bump, often with a central depression. It rarely spreads to other parts of the body.
Squamous cell carcinoma (SCC)
The second most common type, often appearing as a firm, red nodule or a flat, scaly lesion. It can spread to other parts of the body if left untreated.
Melanoma
Melanoma is the most serious type of skin cancer, arising from melanocytes (cells that produce melanin). It can spread rapidly to other parts of the body if not detected and treated early.
Stages of skin cancer
The skin cancer staging helps determine the extent of the disease and guides treatment decisions. The staging system varies slightly depending on the type of skin cancer, but generally includes:
- Stage 0 (In Situ): The cancer is confined to the top layer of skin and has not spread.
- Stage I: The cancer has grown into the deeper layers of skin but has not spread to nearby lymph nodes.
- Stage II: The cancer has grown deeper into the skin.
- Stage III: The cancer has spread to nearby lymph nodes.
- Stage IV: The cancer has spread to distant organs, such as the lungs, liver, or brain.
Specific staging systems
Skin cancer staging is a system used to describe the extent of the cancer's spread within the body. It helps doctors determine the best treatment options and predicts your prognosis.
TNM System
This system is commonly used for melanoma and squamous cell carcinoma , using the size of the tumor (T), involvement of lymph nodes (N), and presence of distant metastasis (M) to determine the stage and the treatment plan.
Skin cancer treatment
At AHN Cancer Institute, you can expect compassionate care and advanced treatment options. We use the latest technologies and therapies, such as mole mapping and immunotherapy. Our skin cancer specialists are with you at every step. We work with you to find the most effective treatment option for your needs.
Fortunately, most skin cancers respond well to treatment. In fact, many basal and squamous cell cancers are very treatable.Melanoma is a more aggressive form of skin cancer that can be life-threatening if left untreated. Our pathologists are skilled in melanoma detection. They are adept at staging and tracking its growth. This level of precision helps your team tailor a treatment option just right for you.




Surgery
Our highly skilled surgeons use the latest techniques and technologies. They collaborate closely with oncologists, dermatologists, and pathologists to determine the best surgical approach for you. Our advanced surgical options include:
- Cryosurgery: This technique uses liquid nitrogen to freeze small, early skin cancer and precancerous lesions called actinic keratosis.
- Excisional surgery: We surgically remove cancerous tissue and a very small area of surrounding healthy skin.
- Curettage and electrodesiccation: This form of surgery involves scraping away layers of cancer cells using a circular blade (curette). We then destroy any remaining cancer cells with an electric needle.
- Plastic and reconstructive surgery: This cosmetic surgical procedure helps restore your appearance after an excessive amount of skin or tissue has been removed.
Radiation therapy and medical oncology
If the cancer has spread, we use advanced treatments to stop or slow the disease’s progression. Your AHN care team will review the therapies and oncology treatments that will work best for your specific case and be the best fit for your needs.
Radiation therapy
We deliver high-dose radiation beams directly to a tumor. Targeting only the tumor minimizes your overall radiation exposure. We are also the only radiation oncology network accredited in western Pennsylvania by the American College of Radiology. This accreditation means AHN meets specific guidelines for patient safety, quality control, and efficiency of equipment. You’re receiving the highest-quality treatment available.
Immunotherapy
We may recommend internal targeted or immunotherapies for more aggressive cases of melanoma including cases of stage IIB/C (deeper or more aggressive appearing melanoma tumor) and stage IV disease (melanoma that has spread to distant organs). Our oncologists are at the forefront of melanoma research and use the newest drug therapies, including new treatments like ipilimumab and pembrolizumab.
Skin cancer FAQs
Skin cancer is a common and often very preventable form of cancer. Despite that, there are a lot of questions and concerns over a skin cancer diagnosis. Your AHN care team is available to help you find answers and solutions. To begin, we’ve included some frequently asked questions that many of our patients have. This information can help you in preparing for conversations with your care team.
What are the first signs of skin cancer?
The first signs of skin cancer often involve changes to the skin. These changes can appear as new growths, sores that don't heal, or alterations in existing moles. Key things to look out for, often summarized by the ABCDEs of Melanoma, include:
- Asymmetry: One half of the mole does not match the other half.
- Border irregularity: The edges of the mole are ragged, notched, or blurred.
- Color variation: The mole has uneven color, with shades of brown, black, tan, white, red, or blue.
- Diameter: The mole is larger than 6 millimeters (about the size of a pencil eraser), though melanomas can be smaller.
- Evolving: The mole is changing in size, shape, color, elevation, or any new symptoms like bleeding, itching, or crusting.
Other general signs can include a sore that doesn't heal, a new bump or nodule, or a scaly patch. It's crucial to perform regular self-skin exams and consult a doctor if you notice any of these signs.
What does stage one skin cancer look like?
Stage one skin cancer most commonly refers to early-stage melanoma, as other types of skin cancer (like basal cell or squamous cell) are staged differently or often not staged in the same complex way unless they are advanced.
A stage one melanoma typically means the cancer is localized to the skin and has not spread to lymph nodes or distant sites. Visually, a stage one melanoma might still exhibit one or more of the ABCDE characteristics mentioned above. It would appear as a mole or lesion that:
- Is asymmetrical, has irregular borders, varied colors, or a diameter larger than 6mm
- Is evolving or changing in appearance
- Crucially, at stage one the melanoma has only grown a certain thickness into the skin (typically less than 1.0 mm, or up to 2.0 mm without ulceration), as measured by a biopsy.
It's impossible to definitively determine the stage of skin cancer based on appearance alone; a biopsy and pathological exam are required.
What can be mistaken for skin cancer?
Many common skin conditions can mimic the appearance of skin cancer, leading to concern. Some of these include:
- Seborrheic Keratoses: These are common, benign skin growths that often look waxy, "stuck-on," and can be brown, black, or tan. They can sometimes have irregular borders or varied pigmentation.
- Atypical (Dysplastic) Nevi: These are moles that look unusual but are benign. While they share some features with melanoma (like asymmetry or irregular borders), they are not cancerous. However, individuals with many atypical moles have a higher risk of developing melanoma.
- Cherry Angiomas: These are common, small, bright red bumps on the skin caused by collections of capillaries.
- Dermatofibromas: These are firm, reddish-brown bumps that often occur on the legs and are benign.
- Pimples, insect bites, or other inflammatory lesions: These can sometimes be mistaken for new growths, especially if they are persistent or develop unusual characteristics.
- Actinic Keratoses: These are precancerous lesions that appear as rough, scaly patches, typically on sun-exposed areas. While not cancer themselves, they can develop into squamous cell carcinoma.
Due to the possibility of misidentification, it is always best to have any suspicious skin issue examined by a dermatologist.
What is the two-week rule for skin cancer?
The two-week rule is a guideline often used in healthcare systems (particularly in the UK's National Health Service, though similar principles apply elsewhere) to prioritize urgent referrals for suspected cancer. For skin cancer, it means that if a primary care physician (PCP) suspects a patient might have skin cancer, particularly melanoma, they should be referred to a specialist (dermatologist or plastic surgeon) within two weeks for further investigation.
This rule is designed to ensure that potential cancers are diagnosed quickly, allowing for earlier treatment and potentially better outcomes. It emphasizes the importance of prompt action when a suspicious lesion is identified.
Contact us
Call the Hope Line at 412-578-HOPE 412-578-4673 to connect with a nurse navigator or schedule an appointment.

